Understanding Iron Deficiency
- Ashley Isabel Tay

- Mar 15, 2022
- 6 min read
Iron deficiency anemia affects more than 1.2 billions individuals worldwide, with iron deficiency in the absence of anemia even more in numbers. In the Global Burden of Disease Study 2016, it is reported that iron deficiency anemia is 1 out of 5 leading causes of living with disability burden and most of all, it is the first cause in women (1). Iron deficiency anemia has significant medical and social impacts such as:
Impairment of cognitive performance in young children (2)
Adverse outcomes of pregnancy for both mothers and newborns (3)
Reduced cognitive ability and reduced productivity at work (4,5)
Cognitive decline in elderly (6,7)
Why do we need Iron?
Iron plays a key role in many physiological processes such as respiration, energy production, DNA synthesis and repair, cell division and myocyte function. (8). Iron is involved in the transportation of oxygen from the lungs to all cells of the body. Iron is also essential for proper cell metabolism and cellular respiration. This element is responsible for preventing cell iron overload that will cause an increase in production of free radicals and lipid peroxidation that can lead to cell death (9).
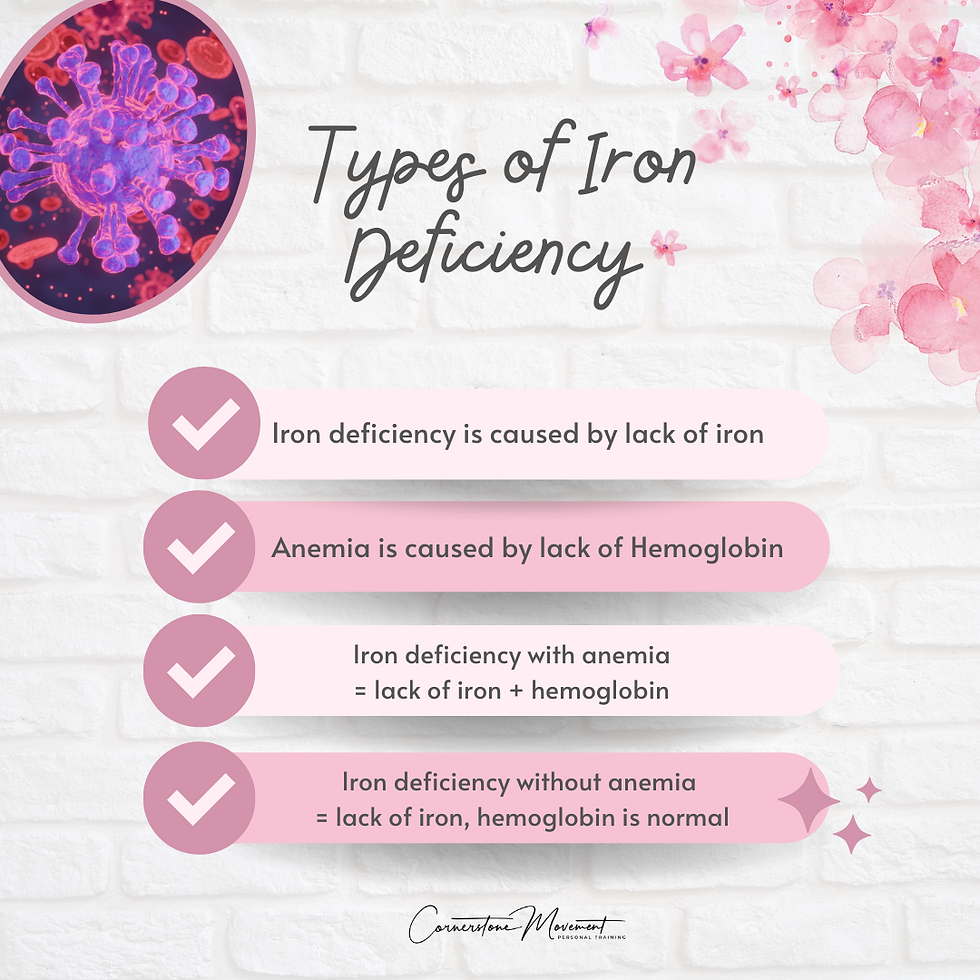
Types of Iron Deficiency (ID)
Additionally, women experiencing heavy menstrual bleeding (HMB) can lead to depletion of iron stores, resulting in iron deficiency (10). Heavy menstrual bleeding (HMB) is defined as the total blood loss per menstrual cycle that exceeds 80mL regularly (11). This prolonged blood loss of more than 7 days in combination with an iron-deficient diet can contribute to the risk of iron deficiency in women (12-14). This is due to women with HMB lose 5 to 6 times more iron per menstrual cycle than women with a normal blood loss on average (15).
Symptoms
Here are the symptoms of iron deficiency to look out for:
(Symptoms of iron deficiency with or without anemia. are quite similar, with anemia experiencing additional alterations of epithelial cells such as dry mouth, cheilitis, atrophic glossitis, Plummer-Vinson pharyngeal webs.)
Iron deficiency with and without anemia can significantly impair quality of life for women (16). However, these impairments can be reversed by iron therapy (17-19). Iron therapy has shown to improve quality of life and physical activity in patients predisposed to iron deficiency due to underlying chronic conditions such as inflammatory disease and heart failure (20-22).
Diagnosis
A correct diagnosis requires laboratory tests. Serum ferritin levels are the gold standard in assessing depletion of iron stores. Serum ferritin levels lower than 15 mg/L reflects exhausted iron stores (23) and in the presence of anemia, ferritin levels are usually lower than 10-12mg/L. In other cases, levels lower than 30 mg/L are considered mild cases. It is important to note that the accuracy of ferritin levels are based in the absence of inflammations or infections.
Treatment
Oral Iron Supplement
Iron salts such as iron sulfate, gluconate and fumarate remain a mainstay of therapy in absolute iron deficiency. The choice of iron compound and administration are largely dependent on clinical status (age, sex, chronic vs recent onset), underlying cause, presence and degree of anemia. It is highly recommended to seek treatment from a healthcare professional to address these issues accordingly.
It is however good to note that there are common side effects of oral supplement such as nausea, vomiting, constipation, or diarrhoea, which may lead to noncompliance with therapy in 30% - 70% of cases(26).
IV Iron
An alternative for patients unresponsive or intolerant to oral compounds is IV iron (27). IV iron has more rapid effect in the body and has negligible gastrointestinal toxicity (26). Also, it preserves the normal microbiome, which would be disrupted by oral iron (28).
However, a concerning issue about IV iron is safety. As iron is a growth factor for several pathogens, iron therapy is contraindicated in infections. Thus, the risk of infection after IV iron is still of controversy and ought to be highlighted to patients.
Overall, we hope this gives you a better understanding of any underlying issues that you are experiencing but yet can't seem to find out the root cause of it. If you do experience any of the above symptoms and is concerned about your iron levels, reach out to us here.
With love,
Ashley
References:
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet, 390 (10100) (2017), pp. 1211-1259
JC McCann, BN Ames. An overview of evidence for a causal relation between iron deficiency during development and deficits in cognitive or behavioral function. Am J Clin Nutr, 85 (4) (2007), pp. 931-945
MM Achebe, A Gafter-Gvili. How I treat anemia in pregnancy: iron, cobalamin, and folate. Blood, 129 (8) (2017), pp. 940-949
Schoep ME, Adang EMM, Maas JWM, De Bie B, Aarts JWM, Nieboer TE. Productivity loss due to menstruation-related symptoms: a nationwide cross-sectional survey among 32 748 women. BMJ Open. 2019;9:e026186.
Cote I, Jacobs P, Cumming D. Work loss associated with increased menstrual loss in the United States. Obstet Gynecol. 2002;100:683–687.
M Falkingham, A Abdelhamid, P Curtis, S Fairweather-Tait, L Dye, L Hooper. The effects of oral iron supplementation on cognition in older children and adults: a systematic review and meta-analysis. Nutr J, 9 (2010), p. 4
M Andro, P Le Squere, S Estivin, A Gentric. Anaemia and cognitive performances in the elderly: a systematic review. Eur J Neurol, 20 (9) (2013), pp. 1234-1240
Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372:1832–1843.
Artym J. Udział laktoferryny w gospodarce z żelazem w orga- nizmie. Część I. Wpływ laktoferryny na wchłanianie, trans- port i magazynowanie żelaza. Postepy Hig Med Dosw. 2008;62: 5 9 9 – 6 11 .
Breymann C, Auerbach M. Iron deficiency in gynecology and obstetrics: clinical implications and management. Hematology Am Soc Hematol Educ Program. 2017;2017:152–159.
Sriprasert I, Pakrashi T, Kimble T, Archer DF. Heavy menstrual bleeding diagnosis and medical management. Contracept Reprod Med. 2017;2:20.
Milman N, Rosdahl N, Lyhne N, Jorgensen T, Graudal N. Iron status in Danish women aged 35–65 years. Relation to menstruation and method of contraception. Acta Obstet Gynecol Scand. 1993;72:601–605.
UK National Health Service. Heavy periods - overview. 2020. https://www.nhs.uk/conditions/heavy-periods/#overview. Accessed May 1 2020
Hercberg S, Preziosi P, Galan P. Iron deficiency in Europe. Public Health Nutr. 2001;4:537–545.
Napolitano M, Dolce A, Celenza G, et al. Iron-dependent erythropoiesis in women with excessive menstrual blood losses and women with normal menses. Ann Hematol. 2014;93:557–563.
Ando K, Morita S, Higashi T, et al. Health-related quality of life among Japanese women with iron-deficiency anemia. Qual Life Res. 2006;15:1559–1563.
Bruner AB, Joffe A, Duggan AK, Casella JF, Brandt J. Randomised study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet. 1996;348:992–996.
Brownlie T 4th, Utermohlen V, Hinton PS, Haas JD. Tissue iron deficiency without anemia impairs adaptation in endurance capacity after aerobic training in previously untrained women. Am J Clin Nutr. 2004;79:437–443.
Yokoi K, Konomi A. Iron deficiency without anaemia is a potential cause of fatigue: meta-analyses of randomised controlled trials and cross-sectional studies. Br J Nutr. 2017;117:1422–1431.
Anker SD, Comin Colet J, Filippatos G, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med. 2009;361:2436–2448.
van Veldhuisen DJ, Ponikowski P, van der Meer P, et al. Effect of ferric carboxymaltose on exercise capacity in patients with chronic heart failure and iron deficiency. Circulation. 2017;136:1374–1383.
Cappellini MD, Comin-Colet J, de Francisco A, et al. Iron deficiency across chronic inflammatory conditions: international expert opinion on definition, diagnosis, and management. Am J Hematol. 2017;92:1068–1078.
WHO . Serum Ferritin Concentrations for the Assessment of Iron Status and Iron Deficiency in Populations. World Health Organization; Geneva, Switzerland: 2011. Vitamin and Mineral Nutrition Information System.
Camaschella, C., 2015. Iron-deficiency anemia. New England journal of medicine, 372(19), pp.1832-1843.
Lopez, A., Cacoub, P., Macdougall, I.C. and Peyrin-Biroulet, L., 2016. Iron deficiency anaemia. The Lancet, 387(10021), pp.907-916.
Tolkien, Z., Stecher, L., Mander, A.P., Pereira, D.I. and Powell, J.J., 2015. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PloS one, 10(2), p.e0117383.
Hershko, C. and Camaschella, C., 2014. How I treat unexplained refractory iron deficiency anemia. Blood, The Journal of the American Society of Hematology, 123(3), pp.326-333.
Lee, T., Clavel, T., Smirnov, K., Schmidt, A., Lagkouvardos, I., Walker, A., Lucio, M., Michalke, B., Schmitt-Kopplin, P., Fedorak, R. and Haller, D., 2017. Oral versus intravenous iron replacement therapy distinctly alters the gut microbiota and metabolome in patients with IBD. Gut, 66(5), pp.863-871.








Comments